My work as a patient advocate and one thing led to many others
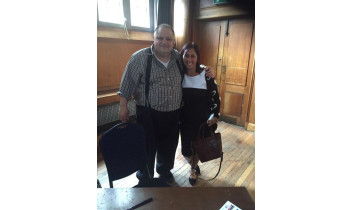
My name is Clara Martins de Barros (pictured here with Steve Silberman, author of Neuro Tribes), I live in London, UK, and I am passionate about patient involvement in healthcare. Here I have answered a few questions in a recent interview with EPAP:
How and why did you become a patient advocate?
I have always wanted to be more proactively involved as a patient advocate, but didn't know how to go about it. It was only when I was a victim of a hate crime a couple of years ago after my move to the UK, followed by a huge disappointing let-down from the counselling services that were meant to be helping with my mental health, and when I started writing to a lot of public and private organisations, that suddenly doors began to open.
I was at rock bottom, and knew that I could only do three things: drown, blame or inspire. So I decided on the latter. As you can imagine, it wasn't that easy or plain sailing. I was alone - I had returned from Portugal after having lived there for a large part of my life - no family or friends nearby, terrified, traumatised, and depressed.
One of the first to contact me was the Institute of Cancer Research (Royal Marsden), where I volunteered in PPI in research, and it was through them that I heard about EPAP. I completed the 7 modules, and then felt better equipped and informed, to start spreading my wings even further.
The significance of this is far deeper than I will ever be able to put into words. It changed my life. It saved my life, really. I will be forever grateful. If you read on, you will see how the learning from those modules is incorporated in everything I do. Since then, EPAP got in touch this year to ask if I would write something for the website.
My life now, little under a year later, consists of having my full time job with my Local Authority and in addition also:
- I am part of a Patient Advisory Group at one of the London hospital’s department of Psychological Medicine & Integrated Care. I have also recently been elected a governor at the hospital.
- I facilitate induction days and give talks about my lived experience with my condition (I'm autistic) as part of Service User Involvement in Training and Education.
- I help at Recovery College, where I have been asked to co-facilitate workshops for the Latin-American Communities in London (in Portuguese).
- I am a member of the Central Commissioning Facility in Patient and Public Involvement Team, which means I am registered with Research for Patient Benefit, the Programme Grants for Applied Research, the Invention for Innovation and the Department of Health Policy Research Programme. I have reviewed and evaluated studies, and this month I am going to be part of a judging panel for a NIHR competition.
- I collaborate and participate in research at the Institute of Psychiatry, where I met healthcare professional Francesca Happe, who is magnificent in research for women with ASCs - Autism Spectrum Conditions. Francesca is someone I admire deeply, and is one of the most down to earth professionals I have met.
- I am also a member of the British Psychological Society, where I try to attend conferences when I can.
- Am a member of the Croydon Autism Partnership Board.
- I am a mentor at work (so other autistic people feel they are not alone and they are worth as much as anyone else), to give training as part of the Employer Disability Confidence Network and recently during 'Learning at Work Week' I gave a talk about being autistic.
What are the main things you have learnt through your work as a patient advocate?
Medicine isn't just about saving lives, it's about changing lives. Being a patient advocate means utilising the skills I have acquired to help others – to give people hope, to inspire. It means the hard work I put into it, is all worthwhile when health professionals and patients alike, come to me and say 'you have taught me things I have never known before, things that no book, lectures or experience, has taught us. Things that have made me realise that my child is not defective, he/she is just different, and now I know more about his/her inside world'. I speak from the heart and combine my empathy with scientific fact.
What are the main challenges of being a patient advocate?
Being autistic means that I am navigating what is a very hostile/alien environment most days, because of sensory overload. As autistic women in general, we are better at performing normative behaviour, which means I have to use even more of my brain's energy to do this, as normative behaviour isn't something that comes natural to us. To manage my energy levels has been an ongoing big challenge for me – especially as I do all this advocacy work on top of a full time job. I get exhausted.
How have you managed to develop relationships with healthcare professionals?
The best and most effective relationships I have developed with healthcare professionals have been when I let my guard down, or when I reveal who I really am. I tell them that if we value originality, and diversity, we must take risks. Because diversity isn't about being compliant, it's about being different, 'sui generis'. I don't look for acceptance, I look for significance.
I'm not afraid of hierarchy or titles. I also suppose in the Autism world, especially in adult autism, relationships with healthcare professionals are easier, there are fewer barriers – there is generally a huge acceptance that you as the person with Autism are an expert of your Autism. Especially as an adult – you often only get access to diagnosis after self-diagnosis, so the Autism service already knows you are well informed about your condition and up to date research on your condition. They expect it and they are very accepting of this.
As a patient advocate I talk to anyone and everyone. When you want to make a difference in the world, you cannot just be like everyone else, you have to be different. So I am just myself, because I AM naturally different. That's when people stop, look, and listen. The journey continues, but the road is less bumpy now.